Periodontal disease is the leading cause of tooth loss in adults. Many dentists recognize dental implants as the preferred method of replacing these missing teeth. However, patients missing teeth because of periodontal disease often have questions about whether implants are an option.
The Importance of Healthy Gums
Firm and pink gums that do not bleed typically indicate a healthy mouth and are essential to a bright smile. Keeping your gums healthy has always been necessary to maintain oral health. However, recent studies have discovered possible links between your gums and your general health.
Your physician often asks you to open your mouth at the outset of a physical exam. Maybe it is because a great deal about your general health can be learned by examining your mouth. For this reason, your oral health has been called a window to your overall health.
Dentists know that healthy gums help you prevent tooth loss, minimize dental implant failure, and avoid premature aging by losing bone around your teeth. In addition to these problems, researchers have now found possible links between gum disease and systemic diseases, such as:
- Cardiovascular diseases.
- Diabetes.
- Bacterial pneumonia.
- Rheumatoid arthritis.
- Pancreatic cancer.
- Alzheimer’s disease.
Although the precise mechanism of how these diseases are linked with periodontal disease is not fully understood, the evidence highlights the importance of oral hygiene and regular dental checkups.
What is Periodontal Disease?
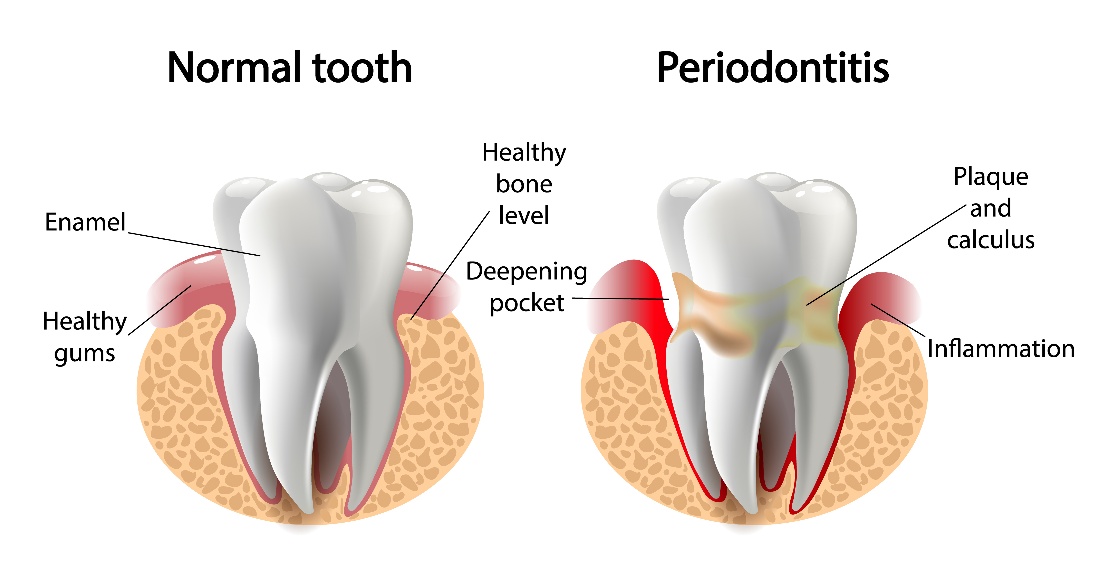
The Centers for Disease Control and Prevention (CDC) reports that almost half of all adults thirty and older have a form of periodontal disease. Periodontal disease begins as gingivitis or gum inflammation in which the gums are red and swollen with possible bleeding. This inflammation is reversible if treated early. However, left untreated, it develops into a more serious gum disease known as periodontitis, commonly called periodontal disease.
With periodontal disease, the gums pull away from their attachment to the teeth and bone. This leaves a pocket alongside the tooth where bacteria continue accumulating, causing an infection that erodes the bone supporting your teeth. As bone is lost, teeth loosen and may require extraction.
Although poor oral hygiene is the chief cause of periodontal disease, other factors can increase your risk, such as:
- Smoking and use of other tobacco products.
- Alcohol consumption.
- Diabetes mellitus.
- Misaligned teeth.
- Heredity.
- Defective dental restorations (bridges, fillings, and crowns).
- Xerostomia, or dry mouth.
- Stress.
- Hormonal changes such as pregnancy and menopause.
- Obesity.
- Compromised immune system.
- Low calcium and vitamin D levels.
- Osteoporosis.
- Clenching or grinding your teeth.
Signs and Symptoms of Periodontal Disease
Although you can have periodontal disease without any symptoms in the initial stages, there are several warning signs, such as:
- Chronic bad breath.
- Gums that bleed when brushing and flossing.
- Tender or painful gums.
- Lingering bad taste.
- Red and swollen gums.
- Tooth sensitivity.
- Loose teeth.
- Receding gums.
- Pain when chewing.
- Change in the way teeth come together when biting.
Can You Get Dental Implants if You Have Gum Disease?
Although dentists prefer replacing teeth with implants, not every patient is an ideal candidate for the procedure. One of the factors that eliminate the implant option is uncontrolled periodontal disease. A successful dental implant relies on a process known as osseointegration, which is the fusion of the titanium implant to the surrounding bone. Untreated periodontal disease involves oral and systemic complications such as unhealthy and infected jaw bone that prevent osseointegration.
When osseointegration fails, the implant loosens and must eventually be removed. Fortunately, most patients can still be considered for implants with the proper periodontal treatment.
All treatments for periodontal disease aim to restore the health of teeth and gums. The specific treatments depend on the severity of the infection and how much damage has occurred. Periodontal treatment can include one or more of the following:
- Professional teeth cleaning. Treating early gum disease (gingivitis) may require only a professional cleaning and polishing to eliminate the inflammation.
- Scaling and root planing. If plaque remains on teeth, it hardens into tartar (calculus). Unlike plaque, tartar requires removal with specialized instruments known as hand and ultrasonic dental scalers. Scaling and root planing removes tartar from below the gum line and on root surfaces. Root surfaces are made smooth to help prevent further plaque buildup.
- Periodontal surgery. Once deep pockets form, you cannot keep them clean with brushing and flossing. Periodontal surgery cleans the pocket and reattaches the gum tissue into a more favorable location. After the surgery, you can prevent the recurrence of periodontal pockets with brushing, flossing, and regular professional teeth cleanings.
- Gum grafting. Healthy gum tissue from one area of your mouth can be taken and grafted to an area damaged by gum disease. This helps protect exposed roots from further diseases, such as dental cavities.
- Periodontal laser treatment. Procedures such as the LANAP protocol can help resolve periodontal disease without surgery. Using laser light, your dentist can gently debride the pocket of bacteria and diseased oral tissues.
- Bone grafting. If you have lost too much bone due to periodontal disease, you may be a candidate for a bone grafting procedure. This is a safe and effective procedure to improve the bone and make implants possible.
These periodontal therapies, combined with consistent home oral health care and regular dental checkups, make dental implants possible for most gum disease patients.
Can You Get Periodontal Disease After Implants?
Unfortunately, you remain at risk of a periodontal disease known as peri-implantitis after having dental implants placed. This condition begins and progresses very much like periodontitis around natural teeth. Primary factors causing peri-implantitis include poor oral hygiene, smoking, uncontrolled diabetes, obesity, and habits such as grinding your teeth or nail-biting.
Although peri-implantitis is the leading cause of implant failure, in most cases, it is preventable. If you practice meticulous oral hygiene, stop smoking, carefully control medical conditions such as diabetes, and avoid parafunctional habits, you can significantly decrease your risk of peri-implantitis.
How To Keep Gums Healthy After Implants
You can take several steps to keep your gums healthy and avoid periodontal diseases such as peri-implantitis. These steps include:
- Brush twice daily with a soft-bristled toothbrush.
- Floss each day with unwaxed tape or special dental implant floss.
- Use a water flosser, like Waterpik, to help dislodge and remove any remaining debris.
- Do not smoke.
- Have regular dental checkups and professional teeth cleanings.
- Stay hydrated.
Schedule an Appointment
Do not let current or past gum disease keep you from inquiring about dental implants to replace missing teeth. Contact us online or call us to learn more about how to prevent further gum disease and discover the benefits of dental implants.